Conference Schedule
Day1: April 25, 2019
Keynote Forum
John F. Inciardi
Touro University of California, USA
Title: Getting a Grip on causal inference in the research setting

10:00-10:40
Biography
John F. Inciardi has lectured extensively at home and abroad on topics related to causal inference. During this time he has developed coursework related to this topic at several universities and has received teaching awards in recognition of these efforts. As a faculty member of the Departments of Pharmacy and of Internal Medicine at the University of California, he has been a long-time mentor to residents and fellows during the design and analysis phases of their health-related investigations. He holds doctoral degrees in both pharmacy and clinical epidemiology.
Abstract
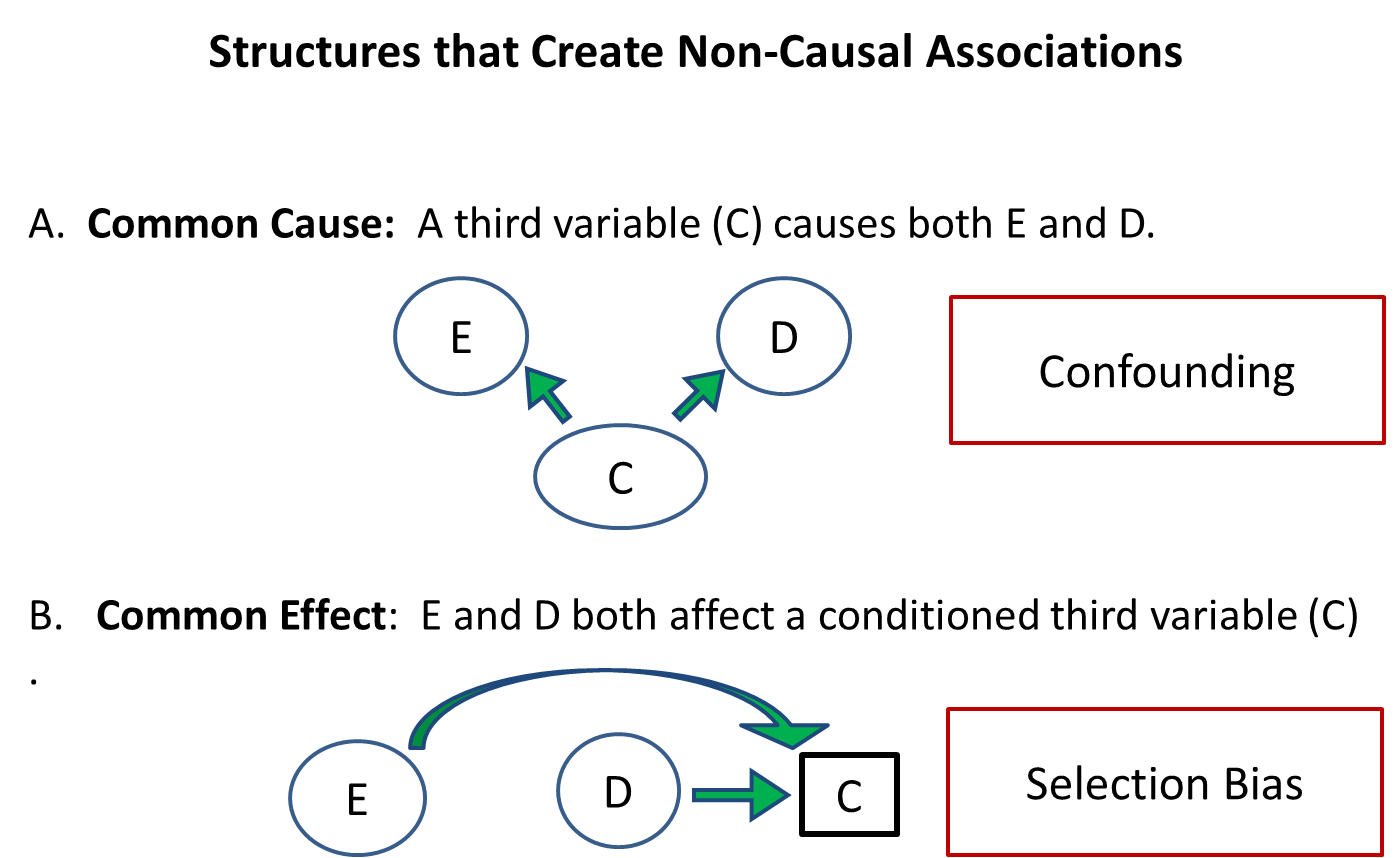
When judging the effects of treatment, health-care providers face the critical task of distinguishing truly causal relationships apart from mere (non-causal) associations. Unfortunately, the task of identifying ‘biasing pathways’ that alter the true effect of an exposure is often a daunting and frequently overlooked adventure. As a result, today’s health-care provider faces a bewilderment of seemingly contradictory reports, some of which appear in highly regarded medical journals.
Epidemiologic studies are commonly constructed around three types of variables: Exposure, outcome and a ‘third’ variable that carries the potential to bias the exposure-outcome relationship. The recent merger of graphical probability theory with established methods for constructing causal diagrams has led to the creation of sophisticated yet highly intuitive tools for establishing causal inference.
This seminar will provide an update on contemporary methods for identifying common threats to the validity of a clinical investigation. The speaker will argue that health care providers by virtue of their education and training are uniquely qualified to provide the expert knowledge requisite for establishing causal inferences. Participants should be able to meet the following course objectives:
- Define confounding from the traditional perspective and from the (modern) structural alternative.
- Identify sources of confounding and selection bias given a directed acyclic graph that accurately conveys the expert knowledge of the investigator.
- Create strategies to adjust or remove biasing pathways responsible for creating confounding and selection bias.
Nicola Brooks
De Montfort University, Leicester, UK
Title: Data changes everything: An investigation into learning analytics to support student success

10:40-11:20
Biography
Nicola Brooks is Associate Dean (Academic) at De Montfort University, Leicester,UK. She is currently completing her Doctorate in Education with the Open University, United Kingdom and is a Senior Fellow of the Higher Education Academy. She is a Registered Nurse who teaches across pre and post registration Nursing courses at De Montfort University. She also works as a freelance clinical trainer for M&K, Cumbria teaching clinical skills and providing professional mandatory updates for both nursing and medical colleagues. Her research interests are related to supporting student success, learning analytics, clinical skills and professional issues.
Abstract
The development and implementation of learning analytics as a mechanism to support student success is an emerging trend within Higher Education. Literature recognises that learning analytics is perceived as an innovative educational development but recognises that little attention has been paid in terms of evaluating its effectiveness or pedagogic usefulness. This research study aims to gain a better understanding of learning analytics to support student success. The research question will broadly examine the opportunities and challenges of learning analytics from a student nurses perspective, and will demonstrate how learning analytics can be successfully implemented within Higher Education.
Through an Interprevist paradigm, this study will draw upon ethnography as a methodological approach to capture unique experiences of student’s nurses and midwives as research participants. Data collected through student focus groups will enable the researcher to gather a broad understanding of learning analytics from those involved and will enable a holistic portrayal of this cultural group.
The main findings of this study can be summarised as the need for learning analytics to have a clear context and purpose within Higher Education to ensure successful development, effectiveness and pedagogic usefulness. Findings demonstrate the need for effective organisational change, academic and student engagement, ownership and motivation. Findings also illustrate disparities (or gaps) with the development and implementation of learning analytics within Higher Education, with disparities needing to be resolved to ensure success. These findings contribute to the increasing evidence base into learning analytics within Higher Education from a unique perspective. Findings show how challenges are overcome to ensure effective institutional adoption and student success. This study will influence future practice by enhancing pedagogic knowledge, increasing understanding and supporting organisational development into this educational development.
Tracks
- Nursing in Emergency Medicine | Professional and Continuing Nursing Education | Critical Care and Emergency Nursing | Nurse Career and Education | Patient Safety & Health Care | Teaching Strategies in Nursing Education | Midwifery & Women’s health | Types of Nursing Education
Location:
Nicola Brooks
De Montfort University, Leicester, UK
Chair
Noelia Ruz Vazquez
Basildon and Thurrock University Hospitals NHS Trust, UK
Title: A review of nursing burnout levels in community nurses and hospital nurses using the MBI (Maslach Burnout Inventory)

11:40-12:05
Biography
She is a registered nurse qualified in 2013 by the University of Valladolid, Spain and working for the NHS in Basildon and Thurrock University Hospital since 2016.
Abstract
Introduction: Nursing burnout has become a paramount object of study in order to ensure the best quality of care to patients and prevent professionals from quitting their job. The aim of this review is to determine if there is any correlation between nursing burnout and the various environments this job is performed in.
Methods: The study design chosen was a literature review, with a qualitative methodology applied. The research consisted of original printing that compared the burnout level between nursing staff in hospital and the community. Publications were searched in databases such as PubMed, CINAHL, LILACS and Cochrane Library, using the descriptors “nursing”, “burnout” and “Maslach”, and employing as Boolean operator “and”. Inclusion criteria were original full text publications written in English and/or Spanish between 2013 and 2018, with a sample over 50 registered nurses who work directly with patient. Some publications were dismissed because they studied the burnout level amongst other medical staff besides nurses, like doctors, paramedics or healthcare assistants. In addition, other printings entirely focused on the nursing practice in specialised areas such as psychiatry, critical care and the emergency department were discarded.
Following this process, the critical reading toll “CASPe” was implemented, acquiring the 11 publications used in this review.
Results: 13 out of the 1057 publications initially found that were related to the research, met the inclusion criteria, and 6 have been included in this review after passing “CASPe”. The results obtained from this review showed that, predominantly, the environment of practice is correlated to burnout syndrome and their prevalence is larger in nurses who work in hospital. Nevertheless, nurses working in hospitals with better work environment reported lowest levels of burnout and it was determined that an increase in the patient-to-nurse ratio is associated with an increase in emotional exhaustion. To this extend, emotional exhaustion was the trait more consistently related to the environment, being the main affected dimension of burnout in nurses who worked in the community.
Conclusions: Environment may affect burnout levels amongst nursing staff, being nurses who work in hospitals more liable than their peers in community.

12:05-12:30
Biography
She is currently coordinator of the Family and Community Nursing Program of the teaching units of the AFYC specialty of Murcia Este_Murcia Oeste and the teaching unit of La Vega Alta, Vega Media del Segura and Altiplano de Murcia (Spain). Recently, in 2018, she completed the Master's degree in the integral management of nursing in DM2, as one of the competencies of the Primary Care nurse. In May she defends his doctoral thesis, at the University of Murcia (Spain). The doctoral research of Doña, María Solé has focused on the work of the Family and Community Care Nurse (AFyC) with the child with obesity and its environment. Her research was based on the interdisciplinary work of a community program led by the AFyC nurse. Currently as coordinator of the Resident Internal Nurses (EIR FyC) program, she is working on improving the resident's assessment based on the competences of the FYC EIR.
Abstract
Introduction: Evaluation and formative feedback are fundamental components of any specialized training teaching program. The resident's book is an appropriate option for conducting formative assessments, particularly for a family and community nursing resident (RIA) whose training includes acquiring many competencies in different rotations across multiple disciplines and in multiple locations. However, the resident book evaluation system has limitations when applied in the current context, since it requires that the competences that must be acquired in each of the rotations be well understood.
Objectives: To detect problems of the current book of the EIR of resident AFyC, and thus to be able to initiate a process to improve its quality and the evaluation of the EIR AFyC.( ínter al nurse resident of family and comunitaria care.) Methodology: Study, descriptive, opinion, using the technique of key informants. Subjects; 24 professionals accredited for teaching (tutors), residents of EFyC, two teaching units, and their Health Centers. A self-report questionnaire with three open-ended questions was sent by email: What are the general problems of the current EIR Book? What are the training problems? What are the problems for the evaluation of the EIR? The data are presented in absolute figures and percentages on the total of responses.
Results: Of the teachers, to whom the survey was sent, they answered a total of 18. They obtained 42 answers to the first question, 31 to the second and 26 to the third question. In total 99 answers, which means an average of 5.5 responses per teacher. Of these, a total of 38 different answers were identified. Of the first question, they were delimited in 14 that correspond to; Competencies (24%), Writing language (19%), use and management (2%), completion time (12%), Repetitions (2%), Extension (2%), Complexity (2%), Competency evaluation (2%), Disawareness (2%), Adaptation to rotations (2%), Consistency with real and daily work (9), Laborious for Tutor (2%), Does not physically exist (2%), Book for Tutor (2%) Of the second question they were grouped in 15; Rotations (29%), Evaluation (6%), Complex and difficult to elaborate (6%), Short duration rotations (6%), Long time (6%), Resident Book Design (6), Little agile (3 %), Tasks (3%), Ignorance (10%), One load (3%), Language (13%), Many criteria (3%), Repetition (3%), Very long (3%), Access ( 3%) and in the third question in 9; Badly defined competences (33%), Extension (15%), Confusing (15%), Adaptation to nursing work (11%), Complex (8%), Difficult use (4%), language (11%), does not evaluate (3%), Procedure (4%).
Conclusion: The answers to the three questions are detected in the main field, the training needs about the resident's book and the comprehension difficulties of the competences of the resident's book. It is surprising that only 8% of the answers refer to the need to improve knowledge about the resident's book. These results can help detect problems in the current resident FYC EIR book and a process can be initiated to improve the quality of the resident's book and the evaluation of the AFyC EIR.
Keywords: Family and Community Care. Specialized Training in Nursing. Resident evaluation. Resident's book
Awatif Alrasheeday
University of Salford- Manchester, UK
Title: A lost human resources, the experience of new graduate nurses in Saudi Arabia
12:30-12:55
Biography
Awatif Alrasheeday is a lecturer at Hail University, Kingdom of Saudi Arabia, Nursing College. Currently, she is a fourth -year PhD candidate at the School of Health Science, Salford University, United Kingdom. Her research interests in exploring the experiences of newly graduate nurses in Saudi Arabia during their first destination posts in a government hospital. In her research, she wanted to have a better understanding of the experience of the new graduate nurse transition, especially in the context of Saudi culture. To do so, she chosen to frame her study by using an ethnographic approach because she consider that NGNs are a specific cultural group. For her PhD Thesis, she is working under the supervision Dr- Joan Livesley and Dr- Neil Murphy. Awatif Alrasheeday aim to critically examine how social and cultural mores were interpreted by NGNs and how they framed and shaped their experiences.
Abstract
Background: Although there is much written about the experiences of newly qualified nurses, this tends to focus on those working in westernised cultures. Less research attention has been paid the experiences of NGN (new graduate nurses) in eastern countries.
Objectives: This study explored, described and interprets the experience of NGNs at one hospital in the northern region of Saudi Arabia. All were in the initial 6 months of their first posts since entering the nursing workforce.
Method: a qualitative case study, informed by ethnographic methods was chosen to conduct the study.
Participants and Sampling: purposive sampling was used to recruit a total of 9 NGNs and 5 senior nurses.
Data collection: Data collection consisted of over 100 hours of fieldwork observations with formal and informal conversations
This data informed one-to-one focused interviews with the participants.
Data Analysis: Data was analyzed using thematic analysis as described by Braun and Clarke (2006) to enable in-depth insight into what was going on and develop a coherent synthesis of the case.
Findings: This work highlights the struggle and challenges that NGNs face in the context of Saudi culture and the drive to modernize the Saudi nursing workforce. The NGNs feel and are treated differently as they struggle to find their place in the structures that frame their working lives.
Margereth Bjorklund
Jonkoping University, Sweden
Title: Cancer patients descriptions of flow experiences

13:55-14:20
Biography
Margereth Björklund is working as a Senior Lecturer at Jönköping University and has completed her PHD in 2010 in the Nordic School of Public Health Gothenburg, Sweden. Her research is about health, health, promotion and empowerment in everyday life with head and neck cancer. Since no knowledge about positive psychology and flow theory in an HNC context exists her current research focuses on this. She works as a Senior Lecturer since 1999 and has been working as a nurse between 1970-2000 in head and neck cancer context. She has published more than 8 papers in reputed journals and has written chapters in books and two books.
Abstract
It is well known that patients with head and neck cancer report many disease- and health-related problems before, during and a long time after completed treatment. A salutogenic focus concentrating on individuals’ strength and health resources has shown to be of significance for experiences of well-being and happiness. This approach of positive psychology moves beyond the disease and support individuals’ growth. When thinking optimistic, the weight places on the individual’s growth and the value of this may create a sense of balance of the problem focused care and research. Mihaly Csikszentmihalyi (1975) claims that where there is a request for enrichment of life, the flow theory is one way. The aim of this study was to describe activities creating experiences of flow for persons suffering of head and neck cancer. With a descriptive design based on a deductive qualitative content analysis reflected on the nine elements of the Csikszentmihalyi flow theory. The participants struggle with everyday problems and fight for finding activities that created flow experiences. They were eager to enjoy trivial things in life. During this process they used unknown skills that increased satisfaction. Mastery, participation, involvement and enjoyment were self-rewarding and created self-care. Good relationships with family, friends and doing things together was central. Individual goals, motivation and skills and feedback from the activities contributing pleasure and happiness. This calls for person-centered care with salutogenic-oriented approaches.
Azahara Torres Santos
University of León, Spain
Title: Training in palliative care and its relationship to coping and attitude to death
14:20-14:45
Biography
Azahara Torres Santos graduated in nursing degree by the University of León (Spain) between 2010 - 2014. When she finished her degree in 2014, she started to work in a nursing home, where she was in charge of 49 residents, in order to acquire professional experience. After one year and a half working there, she decided to try working as a nurse in a different country and moved for a job in an Endocrine and Elderly Care ward in Basildon and Thrurrock University Hospital in UK, and worked there nearly two years and a half. Back in Spain, in her native country, she got a job in the Leon University Hospital where she had her placements during the degree. Currently she is working there in general medicine and palliative care. She do not have any specialization or post graduated master although she studied several post graduated courses to keep me up to date. However, her professional career has been performed mainly on the elderly care field which find rewarding.
Abstract
The nursing staff is in permanent contact with death throughout their working life. In addition, attention in the process of dying, to family members and to the patient, is considered part of the nursing role. Patient care at the end of life generates in the nursing professionals feelings and an attitude to death, as well as a stage of coping with the fact of losing a patient, that are very different among professionals. Objective: To evaluate how a good training in palliative care and teaching techniques of coping with death to nurses, can help these health professionals to cope better with the death of patients and to have a healthier attitude to the patient dying process.
Material and methods: this bibliographical review was achieved through the search of scientific evidence in the PubMed, Google academic, LILACs and Cochrane Library databases of articles in the last five years and the critical reading of them.
Results: The number of articles that relate training in palliative care and coping with death is insufficient to establish scientific evidence. However, articles found that the attitude and feelings to death by nurses are often negative or indifferent. Furthermore, the nurses participating in these studies state that the teaching of coping techniques and training in care palliatives could improve these results.
Conclusion: Training in palliative care for nurses during their university period as well as training throughout their professional career should be greater, so that nurses face better the death of patients and have an attitude that favors better care at the end of life.
Nick Anthony Millar
McMaster University, Canada
Title: Empowering newly-hired nurses through the medicine program orientation workshop: A quality improvement project (MPOW)
14:45-15:10
Biography
Nick Millar is currently the clinical nurse leader in the Medicine Program of the Juravinski Hospital of Hamilton Health Sciences in Hamilton, Ontario, Canada. He is also a part-time lecturer and part-time associate clinical professor in the School of Nursing of McMaster University in Hamilton, Ontario, Canada. His clinical practice areas are geriatric medicine, cardiac medicine, and cardiac surgery.
Abstract
Background: A well-designed on-boarding process for newly-hired nurses (NHN) in acute medicine units promotes patient safety and staff job satisfaction, team integration, and retention. The smooth transition to becoming an acute care nurse ensures that the NHN is successful in learning their new role identity and responsibilities. The inability to ensure this among NHN can result to staff attrition, incremental on-boarding cost, staff shortages, and low morale of existing senior staff.
In 2016, the Juravinski Medicine Program, which has 90-bed capacity, supports NHNs through standardized 5.5-day corporate orientation followed by a 4 to 7 days of clinical preceptorship. The corporate orientation provides general information required to care across different settings in the hospital. Meanwhile, the preceptorship exposes the NHN to the specific clinical practice settings. However, based on feedback from NHNs and their mentors, the current process is lacking in providing knowledge with unit-specific processes and procedures.
Methods: A quality improvement approach was undertaken in the restructuring of the current on-boarding process that will better support NHN. The Meleis’ Transitions Theory (1975) was used as the theoretical model of this work. A working group consisting of management and frontline staff redesigned the current on-boarding process to include (a) 4-hour medicine-specific workshop, (b) protocol for determining number of clinical preceptorship days, (c) visual pathway and toolkit, (d) 7 independent consolidation shifts with assigned nurse, and (e) standardized manager and educator touchpoint meetings.
Results: A total of 62 NHN (31 pre-implementation and 31 post-implementation) were included in the evaluation of this project. Staff self-reported efficacy on medicine unit-specific processes increased from 44% to 82%. Their self-reported preparedness improved from 66% to 80%. The 6-month retention also went up from 56% to 81%.
Conclusion: This project represents the importance of regularly analyzing the on-boarding process so that it aligns with the learning needs of NHNs. It also proves that a smooth transition of NHNs in their new practice environment can promote patient safety through increased efficacy and financial gain through increased staff retention.
Alejandro Fernandez Rufete Millan
University of Valladolid, Spain
Title: Inhalers technique: Trying to find the perfect teaching
15:10-15:35
Biography
Registered nurse qualified in 2011 by the University of Valladolid, Spain. He has worked for the “Servicio Murciano de Salud” in Spain, “CPAS of Charleroi” in Belgium and currently for the NHS in “Basildon and Thurrock University Hospital”.
Abstract
Background: Inhalers are one of the most important resources to treat and control asthma and COPD. The lack of training and follow up, as well as the inability of some patients to perform the right technique, affect their capacity to manage these diseases. The fact that a high percentage of patients make several mistakes when using the inhalers is well known, in this research we try to review the different training methods that can be used to teach individuals the right technique, and we try to find out which one of them count with the higher success rate.
Method: We used a qualitative method to carry out this research, with a systematic review/ meta-analysis design. Five different databases were scrutinised (Pubmed, Cochrane library, Cinahl, Lilacs and Google Scholar) including only clinical trials performed between January the 1st 2013 and January the 1st 2019. The descriptors included in the review were: metered-dose inhaler, dry powder inhaler, education, training program, and method. Using as Boolean operators the words: “and”, “or”.Among the criteria selected to include and exclude publications in this review we chose: original researches, written in Spanish and/or English, carried out in humans having in common as pathologies asthma and/or COPD.
Results: Every selected article points out the alarming amount of mistakes carried out by individuals using their inhalers prior to intervention. Regarding the best teaching method, many papers defend the good results achieved by the traditional face to face training with the healthcare professional, especially if a placebo device or a “flo-tone” are used as example. Follow ups in time show the necessity of an educational support such as videos (internet or DVD) or even summarized labels that avoid people forgetting steps and allow them review the right technique when they need.
Conclusion: The results indicate that a comprehensive educational program including a first training class with a healthcare professional (using devices that allow practice), followed by a support platform of easy access in time for people, will improved the performance of inhaler technique at short and long term.We miss in actual literature this profile of project, which leads us to the conclusion that further investigation in this field is still needed despite the numerous trials already performed regarding inhalers.
Monica RodrÃguez Portela
Isabel I University, Burgos, Spain
Title: The nutraceutical effect of vitamin D against immune systems pathologies
15:55-16:15 (Video Presentation 1)
Biography
Senior student of Human Nutrition and Dietetics at the Universidad Isabel I (Burgos), specialization course in Advanced Clinical Nutrition at Instituto de Ciencias de la Salud y Nutrición, Natural Healing Practitioner at the Escuela Europea Parasanitaria. Currently in an Erasmus+ with Dr. Paolo di Cristófaro specialist in metabolic diseases and eating disorders (Italy).
Abstract
Nowadays, certain natural substances contained in food, are claimed to be beneficial for health. They are called nutraceuticals (NT). Therefore, it is proposed as a general objective to determine vitamin D efficacy as a nutraceutical agent, as well as the effective dose in case of evidence. In order to respond to this objective, a qualitative methodology has been carried out with a bibliographic review study design. The scientific review has been carried out on original studies published during the time period between the 1st of January 2010 and the 1st of January 2019.These studies analyze the therapeutic application of vitamin D and its relationship with the improvement of the immune system. The databases used were: PubMed, Scielo and Cochrane. As descriptors "Decs" were included: nutraceutical, vitamin D3 and immune system. The Boolean operators "AND" and "OR" were used. As an inclusion criterion, it was decided the fact that all the articles must be original and available to full text for free in English and Spanish languages.
On the other hand, we excluded all those studies conducted in a population other than humans or in humans with a sample of less than 30 subjects or with an age lower than 18 years old.
The results of this review have shown that "vitamin D" has a strengthening action of the immune system in different pathologies (acne, multiple sclerosis, infection of the upper respiratory tract or systemic lupus erythematosus) and even in non-pathological but special situations such as pregnancy.
Thus, the analyzed research shows the efficacy of vitamin D supplementation in the general immune system regardless of the pathology and the variables involved, both in small samples (39 subjects) and in large samples (179 subjects). In short treatment (12 weeks) or long duration (52 weeks), with a minimum effective dose of 400 IU / day. After the previous presentation, we can conclude that Vitamin D presents forceful evidence to be recommended in a protocoled way.
Monica RodrÃguez Portela
Isabel I University, Burgos, Spain
Title: Nutritional management and drug-nutrient interactions in the patient with COPD
16:15-16:35 (Video Presentation 2)
Biography
Senior student of Human Nutrition and Dietetics at the Universidad Isabel I (Burgos), specialization course in Advanced Clinical Nutrition at Instituto de Ciencias de la Salud y Nutrición, Natural Healing Practitioner at the Escuela Europea Parasanitaria. Currently in an Erasmus+ with Dr. Paolo di Cristófaro specialist in metabolic diseases and eating disorders (Italy).
Abstract
COPD is one of the most frequent non-transmissible conditions among all respiratory pathologies of a chronic nature. In the United Kingdom, the current prevalence is 27%, causing a high expenditure of healthcare resources with an estimate of £800 million per year.The nutritional situation of the patient suffering COPD is one of the key elements that will determine respiratory failure and it is estimated that between 25% and 40% of patients with COPD are in a state of malnutrition, which is also called "pulmonary cachexia syndrome" (PCS).
This syndrome is characterized by a low body weight, accelerated decrease in fat-free body mass and, in turn, produces high muscle wasting. The objective of the present research was to know the adequate nutritional management of the patient with Chronic Obstructive Pulmonary Disease, as well as the most common drug-nutrient interactions in the treatment of these patients.
In order to respond to this objective a qualitative methodology has been carried out with a review design of the latest available evidence. In addition, the recommendations of the Cochrane collaboration have been followed.The search was conducted in the PubMed, Cochrane, Scopus and Google Academic databases. Also, the publications of the last 8 years (2010-2018) were abided.
The keywords used included the following MESH terminology: pulmonary disease, chronic obstructive pulmonary disease which was linked together, with the Boolean operator AND, as well as the words: nutrition, parenteral nutrition and nutritional support (from the MESH). Among the main results obtained, they emphasize that the nutritional management of these patients constitute a priority in terms of survival; thus, the "pulmonary cachexia syndrome is a factor of poor prognosis, whose survival time ranges from 2 to 4 years in patients with a FEV1 of less than 50% and with underweight.
On the other hand, pharmacological management is complex and food interactions are suggested. Therefore, it is recommended to separate fatty foods from drugs such as theophylline due to the difficulty in its absorption and to require twice the effective dose.
Day2: April 26, 2019
Keynote Forum
John F. Inciardi
Touro University of California, USA
Title: A grand unifying theory of everything true in clinical research

10:00-10:40
Biography
John F. Inciardi has lectured extensively at home and abroad on topics related to causal inference. During this time he has developed coursework related to this topic at several universities and has received teaching awards in recognition of these efforts. As a faculty member of the Departments of Pharmacy and of Internal Medicine at the University of California, Dr. Inciardi has been a long-time mentor to residents and fellows during the design and analysis phases of their health-related investigations. He holds doctoral degrees in both pharmacy and clinical epidemiology.
Abstract
Health-care scientists face a myriad of known and unknown threats that challenge the validity of their research observations. This situation is further complicated by a general misunderstanding regarding the role of statistical analyses when attempting to make causal inferences.
Epidemiologists refer to an invalid association due to improper sampling as ‘selection bias’. Under these circumstances the observed association between an exposure and a putative outcome in a sample of subjects differs from the true causal relationship in the population as a whole (i.e. association does not equal causation).
Identifying selection bias is often a daunting task further complicated by an awkward nomenclature (Table 1). However, recent advances in graphical probability theory have demonstrated that virtually all forms of selection bias can be attributed to a conditioned analysis on a ‘third’ variable (i.e. a variable in addition to those representing exposure and outcome).
This seminar will provide an update on contemporary methods for identifying potential sources of selection bias. The presentation will begin with an overview of bias as product of systematic errors that cannot be discovered through statistical analyses. The speaker will argue that all forms of selection bias are simply the result of conditioning on a common effect of the exposure and the outcome. Participants should be able to meet the following goals:
1. Distinguish statistical association from causal inference when assessing the results of epidemiological research.
2. Describe the elements of a causal structure as they pertain to selection bias.
3. Identify and correct sources of selection bias that commonly complicate the ability to draw causal inference from a research endeavor.
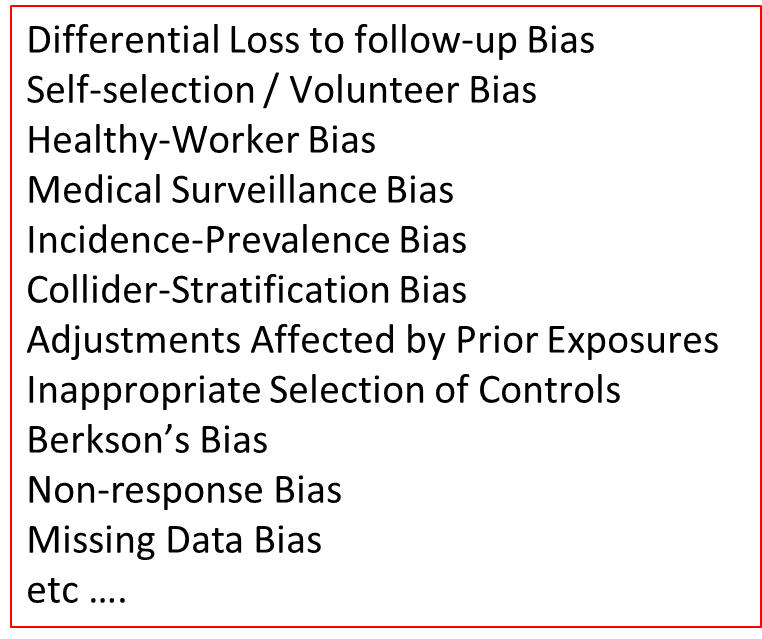
Table 1: A Taxonomy of Selection Bias
Stephen Jacobs
The University of Auckland, New Zealand
Title: Thriving at work as a framework for building highly engaged RNs, motivated and committed to quality patient care

10:40-11:20
Biography
Stephen Jacobs PhD (Medicine) DipTchg BA is a senior lecturer in the School of Nursing at the University of Auckland. He lectures in leadership and management. He is the PhD Advisor and coordinates the Bachelor of Nursing (Honours) programme. He also coordinates the Nurse Wellbeing Project, working in partnership with health providers and School of Nursing academics using research to assist providers develop new management approaches and educational programmes that will support nurses to thrive.
Abstract
This research is the first step in a long-term research programme answering the question: What is the best way to prepare nurses for, and support nurses in, their roles in the nursing workforce so that they flourish in their roles? The School of Nursing delivers a New Entry To Practice (NETP) programme for nurses from different undergraduate providers who are now working in different organisations. Baseline information together with information on the factors that influence intention to leave provides the core information from which a co-design approach is being taken with hospital providers to explore new ways of managing the nursing workforce.
The research follows a strengths-based Appreciative Inquiry (AI) co-design model, working with nurses on the floor and nursing mangers creating a workforce management model that supports nurses to thrive while also meeting the need of a hospital to provide quality service. Nurses at the end of their NETP year, and years two and three after their NETP year, are being asked what aspects of their training and their workplace have supported them to thrive as new nurses, and then what their dream training and support would be.
The benefits of this research will be a greater understanding of training and instructional factors that impact on the ability of early career nurses to thrive. From this basis, further research will work with nurses, educational institutions and health providers to co-create improved systems of training and support that may assist with the thriving and retention of nurses.
LeAnne Young
Memorial Healthcare System, USA
Title: When they cant tell you why it hurts: The importance of implementing a non-accidental trauma guideline
11:40-12:20
Biography
LeAnne Young is the Pediatric Trauma Coordinator at Memorial Regional/Joe DiMaggio Children's Hospital (an ACS verified Adult Level I and Pediatric Level II Trauma Centre) in Hollywood, FL. Her professional career has predominantly focused on the care of the pediatric trauma patient and trauma nursing education. Throughout her 12 years as a pediatric trauma nurse, LeAnne has held leadership positions in trauma program administration, worked in trauma clinical research, and post-acute trauma care management. She is an active member in the STN on the ATCN and Pediatric committees and serving as co-chair of the non-accidental trauma work group.
Abstract
Introduction: According to the Federal Child Abuse Prevention and Treatment Act of 2010, Child Maltreatment is defined as “any recent act or failure to act on the part of a parent or caregiver which results in any of the following: death, serious physical or emotional harm, sexual abuse and/or sexual exploitation” (CAPTA, 2010). Child Maltreatment remains a significant problem in the United States, accounting for over 700,000 reported victims in 2014; resulting in approximately 1580 deaths; an average of 4 deaths each day (Centres for Disease Control, 2014). Proper identification and assessment of victims of child maltreatment is essential for healthcare providers. However, many practitioners and healthcare systems do not have a standardized approach to the identification and assessment process, resulting in variations in management. This is especially true in cases of non-accidental trauma. By establishing a non-accidental trauma guideline, a trauma program can facilitate a standardized process, minimize practitioner bias, and minimize the risk of missing potential victims of abuse.
Objectives: 1. Child Maltreatment remains a significant problem within the United States, resulting in approximately four paediatric deaths each day. 2. The identification and management of patient with suspected non-accidental traumatic injuries requires a systematic approach 3. A standardized non-accidental trauma guideline helps eliminate healthcare provider biases.
Case Presentation/Project Design: Over the course of a year the Paediatric Trauma Program identified several opportunities for improvement in the assessment and management of patents with suspected non-accidental trauma at a community based Paediatric Trauma Centre. During this time there was no established non-accidental trauma guideline. This necessitated the need for the development of a standardized non-accidental trauma guideline to be utilized for patients presenting to the Emergency Department and for direct admission inter-facility paediatric trauma transfers. The development and approval process for the standardized guideline involved a multi-disciplinary approach and took place over the course of eight months. Since the implementation of the guideline there have been no missed injuries in patients with suspected non-accidental trauma.
Discussion/Future Steps/Conclusion: A non-accidental trauma guideline provides a standardized approach to the identification, assessment, and management of patients with suspected non-accidental trauma, and is an essential component in any Paediatric Trauma Program. This type of guideline is equally important in combined programs or in Adult Trauma Programs that also manage paediatric trauma patients. While the development and implementation of a standardized guideline is an important first step, trauma programs must also conduct ongoing monitoring to ensure that the guideline is being followed as part of their performance improvement process.
Tracks
- Types of Nursing Education | Nursing Research and Evidence Based Practice | Future of Nursing Education | Legal Nursing Professional and Continuing Nursing Education | Teaching Strategies in Nursing Education | Pediatric Trauma
Location:
Shelene Giles
FIG Education, USA
Title: Nurse life care planning: Beyond the bedside and into the courtroom

12:20-12:45
Biography
Shelene Giles is a licensed Registered Nurse and her certifications include Certified Nurse Life Care Planner, Certified Life Care Planner, Certified Rehabilitation Counsellor, Medicare Set-Aside Consultant Certified, and Legal Nurse Consultant Certified at Hendersonville, NC, USA. She has extensive knowledge in the specialty practice of nurse life care planning. She holds college degrees in Nursing, Rehabilitation Counselling, Psychology, and Business Administration. Decades ago, her career began in assisting those with disabilities in the community. Her attention moved toward understanding the effects and life-changing events of a catastrophic injury/illness. She discovered the valuable impact of nurses in the litigation settlement process. She specializes in determining future cost of care in catastrophic cases. She provides her knowledge as an expert witness. Between 2007 – 2009, she served on the AANLCP Executive Board as President. She is an internationally recognized speaker/ instructor/mentor/coach and has peer-reviewed publications. She has gained a reputation for being an effective hands-on and compassionate educator.
Abstract
The American Nurses Association (ANA) defines nursing as the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and populations. Nursing is a key element in patient survival as well as in the maintenance, rehabilitation, and preventive aspects of healthcare.
Nurses utilize their education and professional experience to develop a nursing care plan for patients in a medical setting. The nursing care plan and the nursing process have been taken beyond the bedside and into the courtroom. This specialty practice is Nurse Life Care Planning - dealing with individuals who sustained a catastrophic injury/illness resulting in litigation, outlining a plan of care with associated costs, and testifying on behalf of the patient’s needs. Just as the bedside, the nursing process is the foundation of Nurse Life Care Planning.
We are entrepreneurs of a nurse owned business. We have chosen to step away from the bedside – but not step away from our roots as a nurse. We have taken our nursing skills to a higher level. We are the highest paid nurses in the world. We are nurses that specialize in Life Care Planning. Studies show there is a growing need for Nurse Life Care Planners who advocate for patients in the courtroom.
This presentation will explain the specialty practice of Nurse Life Care Planning, define the method of Nurse Life Care Planning, demonstrate the nursing process beyond the bedside, and introduce nurses into an entrepreneurial mindset.
Azahara Torres Santos
University of Leon, Spain
Title: Nursing role in the assessment and nutritional support in oncological patients
12:45-13:10
Biography
Azahara Torres Santos graduated in nursing degree by the University of León (Spain) between 2010 - 2014. When she finished her degree in 2014, she started to work in a nursing home, where she was in charge of 49 residents, in order to acquire professional experience. After one year and a half working there, she decided to try working as a nurse in a different country and moved for a job in an Endocrine and Elderly Care ward in Basildon and Thrurrock University Hospital in UK, and worked there nearly two years and a half. Back in Spain, in her native country, she got a job in the Leon University Hospital where she had her placements during the degree. Currently she is working there in general medicine and palliative care. She do not have any specialization or post graduated master although she studied several post graduated courses to keep me up to date. However, her professional career has been performed mainly on the elderly care field which find rewarding.
Abstract
Cancer is a disease with great importance in the sanitary field due to the high morbi-mortality. Cancer patients have a high risk of malnutrition as consequence of the deterioration of the disease itself and the gastrointestinal effects of the treatment against the disease. A large number of studies have shown that the presence of malnutrition in cancer patients reduces the prognosis, the effectiveness of the treatment as well as the quality of life of these people. There are several tools that allow assessing the nutritional status of the oncological patient before, during and after treatment. The systematic use of these assessment instruments contributes to the rapid detection of patients at risk or with malnutrition, and allows the early implementation of nutritional support strategies to help the treatment and improve the quality of life. The role of nursing in malnutrition related to cancer is crucial at the time of making the nutritional assessment and monitoring of patients during the process.
Objective: To know the different tools for the nutritional assessment of the oncological patient and its effectiveness in the detection of the risk or stage of malnutrition. On the other hand, it is proposed to determine the nutritional strategies based on scientific evidence, that are needed in order to establish care for cancer patients with malnutrition.
Material and methods: This bibliographical review was achieved through the search of scientific evidence in Pubmed, google academic, LILACS and Cochrane Library databases. The search was limited to articles published in the last five years, and its critical reading.
Results and conclusions: The studies reviewed show the existence of several nutritional assessment tools that are effective in detecting and monitoring malnutrition in cancer patients. However, they determine that these instruments are not routinely used in clinical practice, not taking into account the effects of malnutrition on the disease and its treatment. It has been also detected that there are various beneficial nutritional strategies that depend on the individual status of the patients.
Conclusion: Due to the importance of nutritional status in the prognosis and quality of life of cancer patients, it is necessary for health professionals to systematically use the available nutritional assessment tools and apply adequate nutritional support.
Maria Pratt
McMaster University, Canada
Title: A multimodal orientation for clinical nursing instructors

14:10-14:35
Biography
She is currently an Assistant Professor and Faculty Lead for the BScN Accelerated Stream at McMaster University, Canada. Dr. Pratt’s doctoral research focused on the evaluation of unsatisfactory student performance in professional nursing practice courses from the clinical faculty perspective. One of her research recommendations was to develop a multimodal orientation program for novice clinical faculty. She recently completed the Priority Area in Learning and Teaching (PALAT) grant from MacPherson Institute for Leadership, Innovation and Excellence in Teaching based on this research recommendation. Her other research interests include Scholarship of Teaching and Learning in Higher Education, Student Engagement in Large Group PBL and Clinical Lab, and Interprofessional Simulation Learning. Her primary teaching responsibilities are with the undergraduate program. She teaches PBL courses and supervises professional practice students in adult medical-surgical, oncology, and maternal-child practicum settings.
Abstract
There is a growing body of literature on the ‘failure to fail’ unsatisfactory students in nursing and other professional health disciplines. While passing underperforming students can pose serious consequences for patient safety, it can also negatively impact the credibility of educators, nursing institutions, and the nursing profession. Clinical instructors comprise a nursing faculty group that plays a fundamental role in evaluating the learning and development of students. A study at a collaborative undergraduate nursing program in Hamilton, Ontario, Canada revealed that novice and part-time (sessional) clinical instructors tended to pass students who did not achieve course requirements due to personal, professional, and organizational factors associated with failing struggling students. This study further revealed the clinical evaluation process to be emotionally draining for instructors who have failing students.
This current quality improvement project involving a multimodal orientation for novice and part-time clinical instructors was designed to address the clinical nursing faculty concerns that emerged following the study described above.
The multimodal orientation consisted of didactic, interactive, and mentorship experiences to develop faculty members’ skill with assessment and evaluation of unsatisfactory students in clinical practice. Ten novice participants with three or fewer years of clinical teaching experience participated in an initial workshop on the ‘failure to fail’ phenomenon and learned how to support struggling students in clinical practice. Then, over two semesters from September 2017 to April 2018, participants were paired with experienced clinical instructors for mentorship. Participants were interviewed at the end of the academic year about the usefulness of the multimodal orientation. Most participants’ accounts revealed that the workshop helped increase their understanding about managing unsatisfactory students in clinical practice. The importance of assigned mentors in assisting novice instructors to navigate clinical teaching and evaluation of unsatisfactory students cannot be understated. This quality improvement project highlights that providing instructors with knowledge, skills, and mentorship during their early clinical teaching careers can develop their confidence in their evaluative clinical teaching roles.
Maria del Carmen Yuste Bazan
Thurrock Community Team, Spain
Title: Literacy review over sedation in patient with non-invasive ventilation therapy

14:35-15:00
Biography
Maria del Carmen Yuste Bazan obtained her Nursing Degree in Cadiz University (Spain) and after that she studied a Post-Degree in Urgency and Emergency in The European University from Madrid (Spain). Currently, she is working in Thurrock Community Team (Grays) as community nurse. Previously she was working two years in Basildon hospital (Basildon) in an acute respiratory ward as registered nurse, three years in a nursing home (WZC Koning Albert I, Dilbeek, Brussel, Belgium) as registered nurse and nine years in emergency ward in Gregorio Marañon Hospital (Madrid, Spain) as emergency nurse.
Abstract
Background: NIV is a type of assisted respiration consisting on a machine that delivers a positive pressure into the lungs without using an invasive artificial airway in order to obtain effective inspirations. Usually, when the therapy starts the patient could refer symptoms like anxiety or discomfort, triggering agitation and doing the therapy ineffective.
Aim: The aim of this study is to observe if giving sedation previous NIV therapy could enhance the efficacy of this treatment.
Methods: For this investigation, qualitative methodology has been used with a literature review design. The scientific search has been done over originals studies which analyse the benefits to provide sedation before NIV treatment. The analysed database have been Lilacs, Pubmed, Chocrane Library and BVC Portal Regional. Sedation and non-invasive ventilation have been used as descriptors. The period of analysis covered from 1st January 2014 until 1st January 2019. Different selection criteria have been applied.
Results: The articles which have passed the review process show that sedation before NIV is beneficial for the patient, decreasing the usual symptoms and the agitation, therefore, increasing the efficacy of the therapy. Some researches state that one of the adverse effects of the sedation is respiratory depression, however, giving an effective dose has not presented any problems. In addition, the administration of sedation before NIV has shown to be cost effective reducing the hospital admission.
Conclusion: Even though the scientific literature surrounding the subject of this investigation is limited, the current research suggests that the use of sedation previous NIV treatment provides more benefits than adverse effects. However, more investigations are required to provide stronger evidences that support these findings.
Noelia Ruz Vazquez
Basildon and Thurrock University Hospital NHS Trust, UK
Title: Electronic cigarettes as an aid for smoking cessation: A nursing approach to their benefits, risk and health complications
15:20-15:45
Biography
She is a registered nurse qualified in 2013 by the University of Valladolid, Spain and working for the NHS in Basildon and Thurrock University Hospital since 2016.
Abstract
Introduction: Nowadays, smoking is considered one of the most important preventable mortality causes. Smoking cessation in unquestionable beneficial for public health, as it has been proved in several scientific studies, even when some of the techniques used are not completely harmless, such as Electronic cigarettes. Nurses have the duty to keep their knowledge updated, so they can develop their best care. The main objective of this study is to recognise the benefits and risks of E-cigarettes as an effective tool for smoking cessation, so nurses could beneficiate from this information on their daily basis.
Methods: It was employed a qualitative methodology with a literature review as a study design. The research was made about original publications that analyse the benefit/risk of E-cigarettes use against conventional cigarettes, between January 2013 and December 2018. Databases used were PubMed, Google Scholar, CINAHL, LILACS and Cochrane Library. Descriptors “DeCS” used were “vaping”, “lung disease”, “smoking” and “tobacco”, utilizing as Boolean operator “and”. As inclusion criteria, original publications written in English and/or Spanish were accepted, as well as full text publications, studies carried through in humans of both sexes who were over 18, and with a sample over 30 individuals. Several publications related to the topic of study were dismissed due to the realisation of chemical test of diverse substances included in e-cigarettes as lab test. After passing all the selection criteria previously described, a last filter was applied using the critical reading tool “CASPe”, obtaining a total of 8 articles that have been included on this report.
Results: 203 studies were initially identified, but just 21 were considered relevant after screening, and just 8 were eligible after passing CASPe. Overall, the analysed results prove that E-cigarettes are one of the most efficient alternatives to quit smoking without professional support. However, E-cigarettes use is related to more breathing difficulties and more prevalence of COPD and Asthma, compared to non-smokers.
Conclusions: E-cigarettes may be considered as an interesting tool for smoking cessation in terms of risk/benefit if it is compared to other therapies. However, it could not be considered harmless and further research is needed.
Vumilia Bettuel Mmari
University of Dodoma, Tanzania
Title: The implementation fidelity of competency based curriculum for pre service nursing and midwifery programme in Tanzania

15:45-16:10
Biography
Vumilia B. Mmari is a PhD candidate at the University of Dodoma (UDOM) pursuing Doctor of Philosophy in Nursing Education. She is a Nurse Educator completed MSc degree in Nursing Sciences at Muhimbili University of Health and Allied Sciences (MUHAS) in 2010. In 2015/2016 Vumilia joined Tanzania Institute of Project Management (TIPM) for Monitoring and Evaluation Programme. She is now working at the Ministry of Health, Community Development, Gender, Elderly and Children (MOHCDGEC) as a National Training Coordinator for Nursing and Midwifery and Community Health Training Programmes at the ministry’s headquarters in Dodoma, Tanzania. She has been serving as a curricula development expert and training materials designer.
Abstract
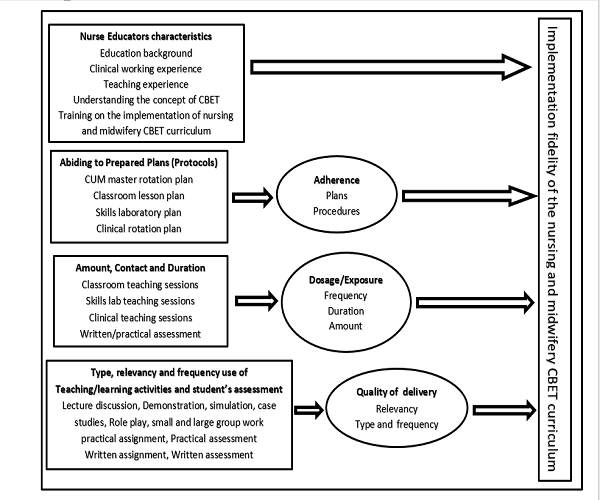
Ten years of nursing and midwifery Competency Based Education and Training (CBET) curriculum implementation the government of Tanzania has made various interventions to support its implementation. Nurse educators were oriented on the implementation of CBET curriculum and training materials, skills laboratories were established and schools were equipped with ICT facilities. Despite all these efforts there is no evidence on how nursing and midwifery CBET curriculum is being implemented since its adaption in 2008 and major revision in 2017. Thus, the balance between the designed curriculum and implemented curriculum is not known. This lack of implementation information greatly limits interpretation of the effectiveness of the curriculum for the intended programme. The aim of this study is to investigate the implementation fidelity of the Pre service Nursing and Midwifery CBET curriculum among nurse educators in Tanzania.
Descriptive cross sectional concurrent mixed method design will be employed, where both qualitative and quantitative approaches will be used to investigate the implementation fidelity of nursing and midwifery CBET curriculum among nurse educators in Tanzania. Population of this study are nurse educators, 215 nurse educators who will be randomly selected to administer questionnaires. In qualitative approach purposeful sampling approach will be used to reach key informants with rich information on the implementation of CBET curriculum for nursing and midwifery pre service programme in Tanzania. Principal of saturation will determine the sample size. Fidelity checklist also will be used to review documents such as CUM master rotation plan, session plans, skills laboratory and clinical rotation schedules.
The modified implementation fidelity conceptual framework will be used to investigate the implementation fidelity for pre service nursing and midwifery CBET curriculum in Tanzania. Four elements (Educators characteristics, Adherence, Dosage and quality of delivery) will be treated together for better understanding of the implementation process for nursing and midwifery programme in Tanzania. Below is the conceptual framework of the study.
Conclusion and significance: There is no information on the implementation fidelity of the pre service nursing and midwifery CBET curriculum in Tanzania. The study will establish the degree of implementation fidelity of the nursing and midwifery CBET curriculum in Tanzania. Furthermore, will provide valid inferences to interpret the effectiveness of the CBET curriculum for the intended programme.
Source: Carrol et al. (2007)and modified by researcher (2018)
Figure 1: Conceptual framework for implementation fidelity of pre service nursing and midwifery CBET curriculum in Tanzania
Fernandez-Ruiz VE
Basildon and Thurrock Hospitals NHS Foundation Trust (United Kingdom) & Murcia University (Spain)
Title: Methodology I2AO2: Cost-effective program led by nursing for the obese patient
16:10-16:30 (Video Presentation)
Biography
She is a Mentor Master Dissertation and Mentor Degree Dissertation at University Murcia (Spain). Working for the NHS, at Basildon and Thurrock University Hospitals, UK, Nurse-Band 5. Collaborator Prof. in Master’s in Health, Women and Care. She is the Member of Organizing Committee: Collaboration in the VII AENTDE Work Days, Redefine the Diagnosis Nurse? Mamma Mia!, UCAM. May in 2009. She had Collaboration in the First National Congress of Nursing UCAM, occupational health and current research, UCAM. May in 2013 and also Collaboration in the Second National Congress of Nursing UCAM, integral and special care Vision Research, UCAM. May in 2014.In April 2018, Collaboration in the 27th Edition Congress Nursing Education & Research. She is the Member of Scientific Committee with collaborations from 2015-2018 such as Collaboration in the XXVI National Congress of Clinical Interview and Communication Assistance. December 2015. Cartagena, Collaboration in the III National Congress of Young Nursing Researchers. December 2017, Murcia and Collaboration in the I International Congress of Young Nursing Researchers. October 2018. Murcia, Spain.
Abstract
Obesity has been recognized as a 21st century pandemic. The frequency of this metabolic disorder has increased during the last decades, causing cardiometabolic complications that imply an increase in the costs of public health services, which has caused it to become a current problem of Public Health. The objective of this research is to design an interdisciplinary program coordinated by nursing to achieve a holistic approach to the obese patient using the resources available from their health center or the community, without causing additional costs to the public health system. A quantitative methodology with a randomized clinical design has been developed. The sample is composed of a total of 74 subjects diagnosed with obesity.
The intervention was a 12-month interdisciplinary program and 1-year follow-up post-intervention. The nurses were present in all activities that were conducted by different professionals and were the link between all professionals and patients to clarify and solve possible difficulties. The intervention conducted by the physical activity and sports sciences professionals consisted of four 40-minute sessions of physical activity every week during the 12 months of intervention (208 sessions in total). Psychologists conducted a 6- minute session of cognitive behavioural therapy on a monthly basis (12 sessions in total). The physician and nutritionist implemented the clinical and nutritional component. They controlled the drug–nutrient interactions and monitored any imbalance or adverse reactions that could occur in response to physical activity and dietary treatment.
The I2AO2programme did not require any economic finance or additional effort from the Healthcare Service of Murcia. This programme was conducted with public resources that were offered to the community and by the support of health care professionals. An interdisciplinary, nurse-led program improves participants cardiometabolic and psychological health, while maintaining long-term effects. The results obtained have shown that cost-effective programs can be achieved for patients. The nurse had an important role in our interdisciplinary program as a nexus between the patient, different professionals and the community.


